Preterm Premature Rupture of the Membranes (PPROM)
What is it, what should you know, how can it impact you emotionally and stories of hope.
This month is PPROM (or PROM) awareness month, PPROM stands for Preterm Premature Rupture of Membranes, which refers to a pregnant person's waters breaking prematurely, before labour and before 37 weeks gestation, leading to the potential for needing neonatal intensive care (NICU).
There are many parents within the neonatal and birth trauma community who experienced PROM and I thought it was important to talk about what it is, what you should know, how it can impact you emotionally or psychologically, from the point of view of a Clinical Psychologist and share some stories of hope from others who have been through it.
What is PROM?
Premature rupture of membranes (PROM) refers to the breaking or tearing of the amniotic sac, which contains the fluid (the waters) that surrounds and protects the developing baby during pregnancy. Typically, the amniotic sac ruptures during labor, leading to the release of the fluid, commonly known as the "water breaking." However, in the case of PROM, this rupture occurs before the onset of labor before 37 weeks, which is why it is considered premature.
There can be various reasons why PROM happens. Some of the common causes include:
1. Infections: Certain infections in the reproductive tract can weaken the membranes, making them more prone to rupture prematurely.
2. Weakened membranes: In some cases, the amniotic sac may be weaker than usual, making it more likely to rupture early.
3. Preterm labor: The uterus may start contracting and put pressure on the amniotic sac, causing it to break before the due date.
4. Cervical incompetence (not a very nice name!): A condition where the cervix (the lower part of the uterus) is weak or unable to stay closed, leading to early rupture of the membranes.
5. Multiple pregnancies: Women carrying twins or multiples have a higher risk of PROM compared to those with a single pregnancy.
6. Previous history: If a woman has experienced PROM in a previous pregnancy, she may have an increased risk of it happening again. They may utilise something called a “cervical stitch” in following pregnancies to reduce the risk of it happening again.
7. Unknown reasons: Sometimes, there isn’t an answer as to why a persons waters have broken early, which can be difficult to sit with. Premature rupture of membranes can occur spontaneously without any apparent cause.
We asked our NICU community what they wanted people to know about PPROM, this is what they answered:
Losing your waters does not necessarily then mean imminent birth. You can loose your waters whilst your baby is a premature gestation and still get to full term. Losing your waters does not equal labour.
Trust your instincts, advocate for yourself, some medical professionals may mistake your waters for urine, you know your body best.
Your body can experience a partial rupture of membranes, meaning that there isn’t a “big gush” like you see in the movies.
Always get checked if you are unsure
It can happen to anyone
It can be that things need to move quickly, or the medical team are able to help you slow things down to keep your baby in longer, it depends on your body and how your baby are
Often, medical teams do not know why it happened
It is not your fault, your body is not to blame
How may this experience impact you emotionally?
PROM can have a significant psychological impact on pregnant people and their partners, I wanted to explore what some of the main feelings may be:
1. Anxiety and Stress: PROM can lead to heightened anxiety and stress due to the uncertainty and potential risks associated with preterm birth. They may worry about the health and well-being of your baby, potential complications, and the overall outcome of the pregnancy. The anxiety is something that can persist after coming home with your baby, as the overwhelming stress can almost “get stuck” after your birth and potential neonatal stay.
2. Emotional Rollercoaster: Dealing with PROM can result in emotional ups and downs, as you would absolutely expect. Individuals may experience a range of emotions, including fear, sadness, anger, frustration, and hopelessness.
3.Struggling with uncertainty: There is a huge element of sitting with uncertainty during PROM, meaning that you do not know what is going to happen and when. It can feel difficult to know what to do, what is going to happen. You may find yourself searching for answers, either on google, or guessing, worrying or ruminating, or even blaming yourself to create a feeling of certainty.
4. Loss of Control: PROM can make individuals feel a loss of control over their pregnancy and birth experience. The rupture of membranes often means that the baby will be born prematurely, and the timing and circumstances may be out of their hands. To help people feel more in control, they will often do certain things that allow them to feel safe, so whether this is enhanced checking, reassurance seeking, monitoring, ruminating, avoiding… the list goes on. It is common to try and overcompensate with “control” strategies to reduce the feelings of being out of control, which can feel intolerable for many.
5. Self Doubt: When your waters go early, there can be a huge element of self doubt, I have heard people talking about thinking that they have wet themselves, or even doubting what they are feeling if they have gone into early labour. This further gets complicated, when hospital teams have then reinforced this belief and have told people they are not in labour, or not taken them seriously, when this is what their truth was. It is really hard to believe yourself, but trust that you know your body best. If something doesn't feel right, it often isn't.
6. Anticipation and Hope: Despite the challenges, individuals may also experience moments of hope and anticipation. They may look for positive stories, support, and information to help them navigate through the situation. Connecting with others who have gone through similar experiences, such as through blog posts, can provide a sense of community and reassurance.
7. Decision-Making and Uncertainty: PROM may necessitate making difficult decisions, such as the timing of delivery or medical interventions. The uncertainty surrounding the situation can make decision-making more challenging, and being in fight, flight, freeze, fawn mode (survival mode) can also make it more difficult to advocate, make decisions and utilise your logical brain at this time.
8. My body failed: I often hear people in therapy saying “I should have kept them in longer.” “I should have done more.” “My body had one thing to do.” Again, this is incredibly common, people often place blame on themselves, their body and their ability to parent as a result of PROM. This self blame almost feels more tolerable than sitting with uncertainty, so it has a function. However, it is often not true. It is not your fault, you did not do anything wrong.
9. Missed moments: As with all premature birth, there is often a feeling of missed moments, grief for how you feel it should have been. It is a very real grief that can make you feel angry, sad, jealous, robbed and disconnected.
It's important to note that the psychological impact of PPROM can vary from person to person. Some individuals may find strength and resilience in coping with the situation, while others may struggle more significantly. Seeking support from healthcare professionals, joining support groups, or reading blog posts written by individuals who have gone through similar experiences can help individuals manage the psychological impact of PPROM. If you feel like you need more support, please contact me, I would be happy to talk to you.
Laura’s Story
Laura has kindly agreed to share her story of having PPROM and preterm labour during her twin pregnancy.
Laura says:
“I was pregnant with MCDA twins from Northern Ireland, we were diagnosed with TTTS (Twin to Twin Transfusion Syndrome) and SIUGR (Selective intrauterine growth restriction), I had laser ablation surgery at 19 weeks in London. The risks of surgery are PPROM and preterm labour.
My waters broke in a massive gush while I was working, I immediately went into a panic and rang the foetal assessment unit as I was only 22+6weeks. My partner rushed me to the hospital, trying to save them but I knew if I was in labour we were going to lose them. They confirmed my waters had broke around twin 1 but I was not in labour, although it was likely I'd give birth in a week.
The doctors gave detailed descriptions of what 23 week babies are like and success stories were rare. I was sent to our higher level hospital but they had never had a set of 23 week twins survive. Our smaller twin weighed 260g, if I went into labour it was unlikely she would survive and if she did they could only offer comfort care. Our bigger twin was 450g and we were told she had more of a chance but it was unlikely either would survive. My partner was optimistic. The only question I could only ask was if the babies would feel any pain. I spent my birthday wondering if I would be cradling my babies at the end of it.
I was separated from my family, my 2 year old son and ripped from my life. I had nothing to do but think about my babies and how the odds were against us. I was on a postnatal ward surrounded by new babies, the pain was unbearable. My son was unable to visit me for a few weeks due to lingering covid restrictions, and finally they made an allowance for him. I video called him daily but my heart was broken, I felt like I had abandoned him. My waters continued to leak the entire pregnancy, which itself is mentally challenging.
As the weeks progressed the doctors became more optimistic, our smaller twin was in trouble at 25 weeks and we thought again we would lose her. I was scanned daily and things did eventually improve. At 28+5weeks I started bleeding and the twins were delivered via emergency c section due to partial placenta abruption and TAPS. They weighed 2lb9oz and 1lb7oz and spent 9 and 12 weeks in NICU respectively. I returned to the postnatal ward I had spent 6 weeks on, no longer pregnant and without my babies. I discharged myself as soon as I could. I travelled daily to see the twins fight for their lives.
Prior to PPROM I didn't know you could stay pregnant once your waters broke, our babies continued to make waters, they both came home off oxygen. Despite the odds our babies are thriving at 8 months old now.”
Vicki’s Story
“My daughter’s birth story is one I talk about freely. It is important to me to discuss what it means to go into labour prematurely, because it’s something I was not prepared for or really aware of. The more people tell their story, the more other mum’s will hopefully feel less alone if it ever were to happen to them.
So here goes. I went into labour at 32 (+2) weeks pregnant, while away for my Dad’s birthday in the very rural part of North Wales. If it wasn’t for one of my best friend’s telling me (honestly) about her labour I would have had no idea I even needed to call the midwife straight away. It was the middle of the night and I woke up to what I thought was me wetting myself a little bit, I convinced myself that was all it was (changed my underwear) and went back to sleep. Then a couple of hours later it happened again and I realised this wasn’t me losing control of my bladder but was in fact my waters leaking ... I called my local emergency out of hours midwife number and was advised to search for hospital’s in the area that had a maternity ward to be checked over (this happened to be a 50 mins drive away from where we were staying). On the way to the hospital, driving at 5am along unknown country roads, I started to get what felt like period cramps but was still in complete denial thinking (and discussing with my husband) that I would just need a course of injections to stop the leaking and then we’d be back at the holiday cottage later on that day, maybe worst case the next day. On arrival at the hospital the Dr who checked on me, told me she just wanted to check “down there” to make sure everything was ok. That’s when my world turned upside down, when she said the words “I can see hair, you are 4cm dilated, you are definitely having your baby this weekend, we need to do what we can to delay labour and keep your baby inside for as long as possible” (she may have said more than this to soften the news but these are the snippets I took and remember from that day).
I’m not sure how quickly after she said those words I was sick, but it felt like straight away (I realise now looking back it was a shock reaction). I was given a steroid injection soon after being admitted to help my baby’s lungs, was put on strict bed rest to prolong labour and as a precaution was nil by mouth. During my labour I was advised that due to my gestation there would be a lot of staff in the delivery suite, some for me, some for my baby. I was advised at my gestation, my baby would be 3-4lbs and may not be able to breathe unaided. The hospital wasn’t equipped to care for babies who needed intensive or high dependency care, so there was a chance my baby would have to be transferred (leaving me behind). My mum (who was my birth partner, as well as my husband) had driven nearly 4 hours to get to me only to be told the hospital had a Norovirus outbreak so was not allowed to enter the hospital, luckily my husband was with me when I was admitted otherwise I would have given birth alone. Sooner than the medical staff wanted (they wanted to give me 2 steroid injections, 6 hours apart, but due to the speed of my Labour only gave me 1), my daughter was born at 32+2 weighing 5lbs exactly. I held my breath without realising, while she took her first breath unaided, to the delight of all in the room. She surprised us all from the beginning and as a wonderful 5 year old she continues to wow us every chance she gets.
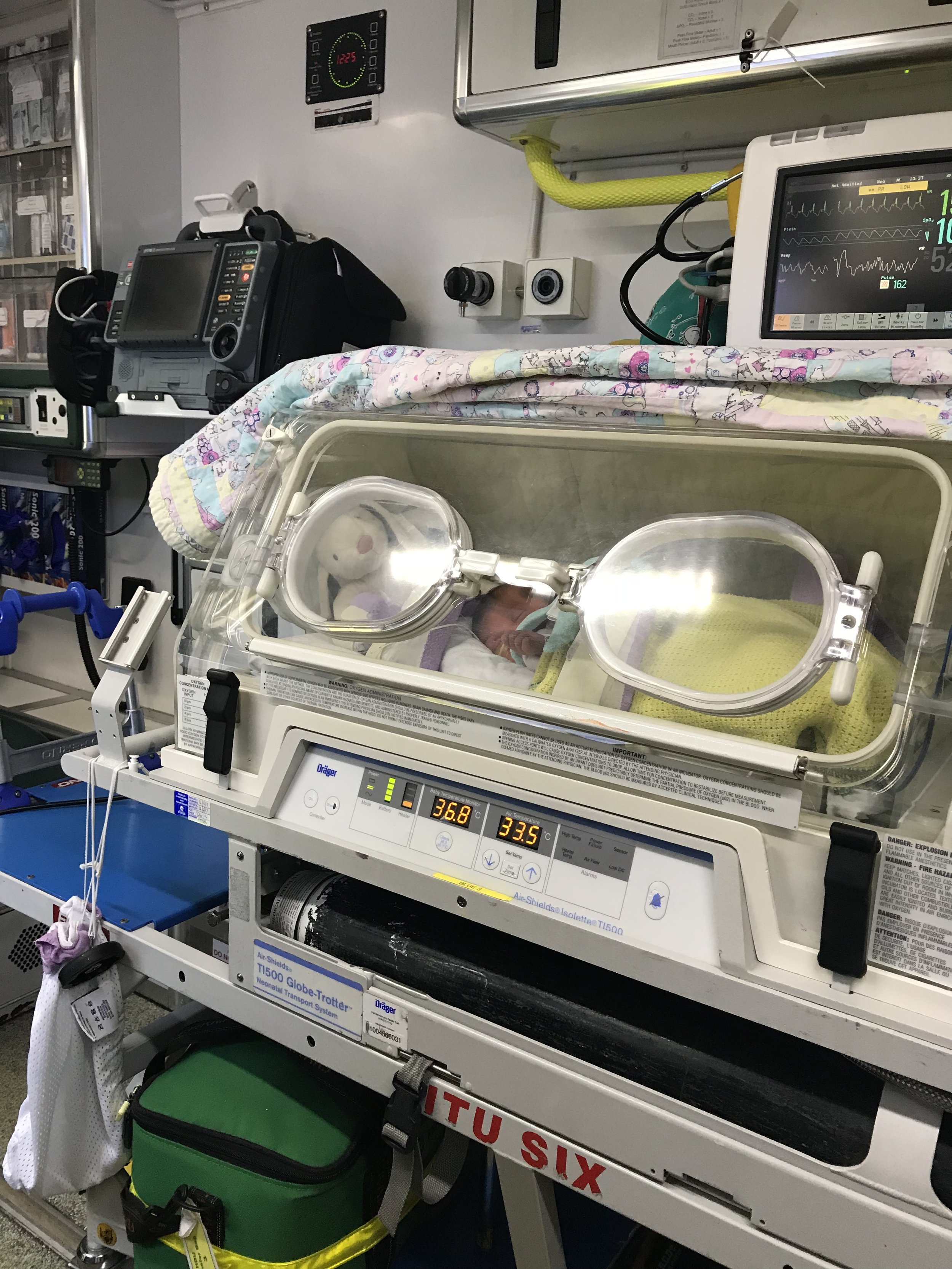
Having preterm premature rupture of the membranes (PPROM) was terrifying. It made me feel like my body had failed my baby. As a mum you are meant to grow your baby and keep it safe in your womb for 9 months, I was not able to do that. I felt like having PPROM and giving birth prematurely, I missed out on many things ‘normal’ pregnant women get to experience, including the Labour I wanted and the new born experience. My first night after Labour my bump was empty and so was the space next to me on the ward where she should have been. My baby was in an incubator, in an ambulance, being transferred to my local hospital at 2 days old, not at home with me enjoying skin to skin new born cuddles. The first 3.5 weeks of her life all she knew was a hospital not her home. Now I have had another baby and have been monitored under a consultant, it was picked up that my cervix was shrinking and I was prescribed progesterone to prevent further shrinkage. This may have been the cause of PPROM with my first pregnancy but I will never know. I’m glad I had a friend explain to me the waters can trickle and not just gush like they do in movies!”
Thank you so much to Laura and Vicki for sharing your stories with us and helping others feel less alone.
For further support about PPROM please see:
Please contact me for individual therapy, EMDR, couples support and group support.